How AI Is Transforming Claims Handling
Stay ahead in support AI
Get our newest articles and field notes on autonomous support.
The first report of a loss, whether it’s a burst pipe, a minor accident, or a theft, shapes how policyholders view the entire claims experience. This moment carries disproportionate weight in shaping customer loyalty and retention. Data shows that 68% of customers say their satisfaction with a claim is shaped more by the FNOL interaction than by the final payout or their relationship with the adjuster, because it happens when they need help most.
Traditional FNOL often falls short. Customers face long hold times, repeat their story to multiple agents, and are told to wait days for callbacks while their problems remain unresolved, leaving them feeling abandoned and remembering the experience at renewal time.
AI FNOL automation changes this by enabling instant claim intake across channels, real-time policy checks, smart routing based on claim details, and proactive updates throughout the process. Insurers that automate FNOL stand out from competitors still dependent on manual workflows and overloaded call centres.
What is FNOL and Why Does It Matter in Insurance?
First Notice of Loss (FNOL) is the initial report a policyholder makes after an incident, sharing event details, verifying that coverage applies, and initiating the claims workflow that will lead to resolution. The definition sounds easy, but the operational reality is complex.
The policyholder is stressed, possibly scared, and hoping that years of premium payments bring genuine support when needed most. They may deal with a damaged vehicle, watching water pool across their floor, or realizing valuable property has vanished. How insurers handle this moment determines whether customers feel supported or abandoned when they need help most.
What Are Common Challenges with Traditional FNOL Processes?
The most common challenges of traditional FNOL include manual data entry, slow processing, and routine errors. These challenges are structural, embedded in decades of manual intake processes that create unnecessary friction and cost.
Representatives taking notes from phone conversations achieve good accuracy during slower hours, but performance degrades during high-volume periods. Errors cause downstream problems, including reassignments when claims reach the wrong team, coverage disputes when policy details are incorrect, and frustrated callback requests when customers must correct information they already provided.
Intake can take days when customers can’t reach agents, agents lack the right information, and routing requires manual review. Storm surges, holiday periods, and product recalls overwhelm call center capacity, leaving customers on hold for extended periods or abandoning calls and creating duplicate records when they try again later.
Claims assigned to the wrong team sit in the queue until someone reviews, recognizes the error, and reroutes them to the appropriate destination. Days vanish while customers receive no communication and wonder whether anyone is working on their claim. Frustration grows when customers call for updates and reach agents who can’t see information held by other teams..
Why Broken FNOL Negates Other Claims Investments
Carriers have invested heavily in claims systems, adjuster training, fraud detection, and settlement automation. These investments underperform when FNOL is broken, because no downstream process fixes poor intake data. Even the best claims workflow delivers poor results if it starts with incomplete or inaccurate information.
This makes FNOL transformation one of the highest-ROI improvements in claims operations, yet many insurers still focus on downstream optimization while neglecting the intake process that determines the quality of everything that follows.
How Does an Optimized FNOL Process Work?
An optimized AI-powered FNOL process follows a sequence where each step builds toward complete claim initiation rather than merely capturing information for later human processing. The distinction matters because platforms that resolve intake deliver different operational results than platforms that simply digitize data collection.
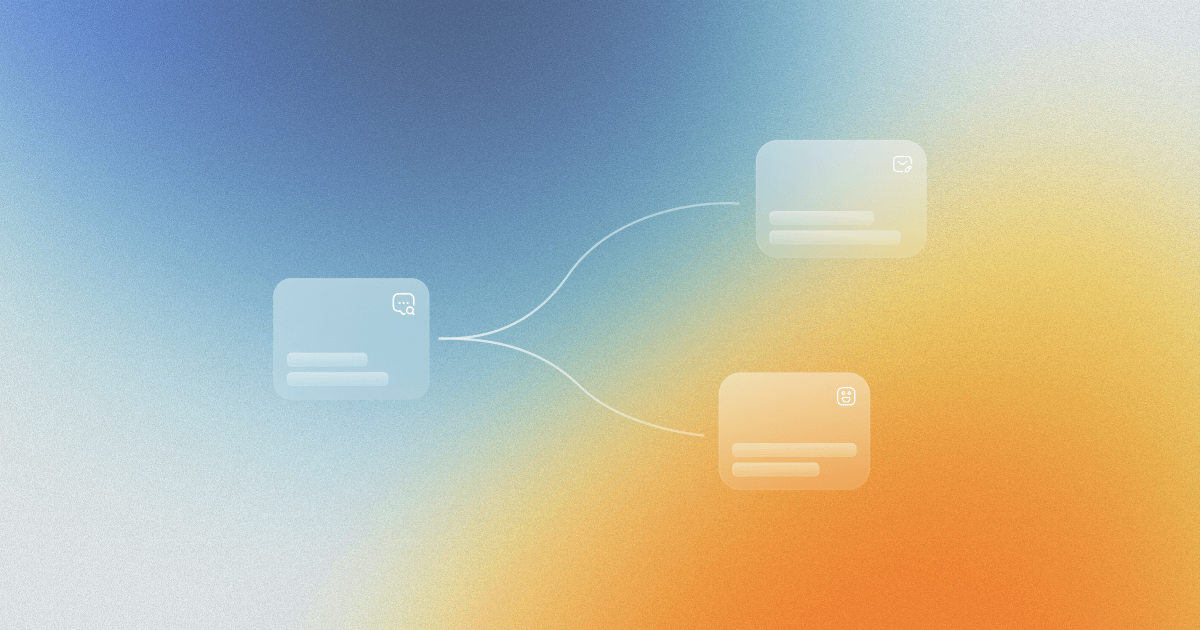
Modern FNOL systems operate through a fully integrated workflow where intake, validation, routing, and communication happen simultaneously rather than as separate sequential steps. Claims arrive through customers' preferred channels before the system immediately extracts structured information using NLP for voice and text, OCR for documents, and computer vision for damage assessment while validating policy details and flagging missing information during the initial interaction rather than days later.
Claims meeting straight-through processing criteria route directly to automated resolution, medium complexity cases land with appropriate adjusters based on claim type, severity, workload, and skill matching, and complex claims triggering fraud or compliance flags escalate immediately with full context.
This automated triage eliminates dispatcher bottlenecks while proactive status updates, appointment scheduling, and document requests flow automatically through customer-preferred channels, reducing inbound inquiry volume and eliminating the need for customers to chase updates.
Technologies Powering AI FNOL Automation
The technologies that power FNOL automation involve AI and machine learning, NLP, IDP, OCR, damage assessment, and voice AI. Understanding these helps with vendor evaluation, since not all platforms offer the same capabilities, and quality varies widely. The key technologies driving modern first notice of loss automation include:
- Artificial Intelligence and Machine Learning - Handle claim type classification, severity scoring, fraud probability assessment, and routing optimization while continuously improving from production data and adapting as claims patterns shift over time
- Natural Language Processing - Extracts structured data from unstructured customer descriptions, enabling natural conversation during intake and capturing relevant details like incident type, damage description, involved parties, location, and timeline from conversational input
- Intelligent Document Processing and OCR - Ingest police reports, medical records, repair estimates, invoices, and damage photos, extracting relevant fields to populate claim records automatically while handling handwritten notes, multi-page documents, and non-standard formats with high accuracy
- Computer Vision for Damage Assessment - Analyzes damage photos to identify affected components, classify damage types, gauge severity, and generate preliminary damage estimates during FNOL, enabling faster reserve setting and more accurate adjuster assignment
- Voice and Conversational AI - Handle phone intake through natural conversation without hold times or capacity constraints, understanding context, remembering previous information, adapting responses based on claim circumstances, and detecting caller's emotional state to adjust tone appropriately
What Are the Benefits of Automating FNOL?
Automating FNOL brings six notable benefits, from faster claims initiation, through improved data accuracy, enhanced customer experience, and cost reduction, to early fraud detection and scalability.
Faster Claims Initiation
One carrier cut acknowledgment time from over four hours to under ten minutes with FNOL automation, and the speed gains carried through assignment, investigation, and settlement. Faster initiation means adjusters begin work sooner, investigations launch with less delay, and settlements reach customers more quickly.
Improved Data Accuracy and Claim Quality
Insurers using strong automation reach 95 to 98 percent accuracy on standard requests compared to 80% for manual processes, enabling downstream automation that fails without consistent input data. Higher accuracy reduces rework, prevents routing errors, and ensures coverage determinations and reserve calculations start from correct information. The data quality improvement ripples through every subsequent claim stage.
Enhanced Customer Experience
One agency achieved an 18-point NPS increase after automation rollout, with digital FNOL users outscoring traditional phone intake on satisfaction surveys. Customers appreciate speed, transparency about claim status, and control over their information rather than dependence on callbacks and hold queues. The experience improvement drives retention benefits that enhance the customer lifetimes.
Cost Reduction and Operational Efficiency
Comprehensive automation can cut claims processing costs by up to 70% - by reducing call centre demand, removing manual data entry, and avoiding the rework caused by human error. Cost reduction enables either margin improvement or reinvestment in customer experience enhancements.
Early Fraud Detection
Scoring algorithms flag suspicious patterns as claims arrive rather than days or weeks later, when investigation resources are already invested. Early detection prevents resource waste on fraudulent claims while enabling faster processing for legitimate claims that clear fraud screening quickly.
Scalability During High-Volume Periods
AI scales without staffing lead time, training requirements, or overtime costs, absorbing hurricane surges, wildfire events, and product recall spikes without quality degradation or service delays. Carriers in catastrophe-exposed regions particularly benefit from automation that handles volume fluctuations gracefully.
How to Implement AI FNOL Automation: Getting Started
Implementing AI FNOL automation happens in five steps, starting with mapping the existing FNOL process, identifying gaps, evaluating technologies, verifying integration, and piloting. Here’s how each step goes:
Step 1: Map Your Current FNOL Process
Document existing workflow details, including channels accepted, data elements captured at each stage, validation methods, routing logic, manual labor concentration areas, and error frequency by type. This baseline enables measurement of whether automation delivers expected results.
Step 2: Quantify Gaps and Pain Points
Measure current problems with specific numbers. What share of claims need post-intake correction? What's the average hold time during surges? How many claims misroute on initial assignment? What percentage of customers call back to provide missing information? These metrics reveal where automation creates impact and establish clear success targets.
Step 3: Evaluate Technologies and Vendors
Assess whether platforms complete intake end-to-end or simply collect data for human processing. Examine integration depth with existing policy administration, claims management, and payment systems. Determine whether vendors understand insurance-specific requirements, including regulatory compliance, coverage logic complexity, and claims workflow nuances.
Step 4: Verify Integration Capabilities
Confirm that platforms can execute actions across policy admin, claims, and payment systems rather than just reading data. Read-only integrations provide limited benefit since manual handoffs remain necessary for claim creation, assignment, and payment. True straight-through processing requires execution capabilities across the full technology stack.
Step 5: Start with a Pilot
Select one claim type, channel, or region to prove results before expanding. Monitor cycle time, accuracy rates, routing correctness, and customer satisfaction throughout the pilot period. Learn from results and adjust the configuration before systematic expansion.
What Makes an AI Tool Right for FNOL?
The right AI tool for FNOL resolves claims instead of basic intake, provides omnichannel capabilities, leverages insurance-specific AI, integrates with existing systems, scales as the needs grow, and embraces the time-to-value metric. These features help executives properly research and choose the right FNOL software.
True Resolution vs. Basic Intake
Distinguish between platforms that queue captured data for human processing and those that complete intake autonomously by validating coverage, setting preliminary reserves, creating claim records, assigning adjusters, and sending confirmations. Clarify exactly what happens without human involvement versus what requires manual steps.
Omnichannel Capabilities
Verify that platforms truly unify channels rather than offering disconnected intake paths. Claims started on mobile and continued by phone should flow seamlessly with full context preserved, not force customers to repeat information when switching contact methods.
Insurance-Specific AI
Insurance-built AI customer service platforms include policy structures, coverage logic, regulatory requirements, and claims workflow knowledge from initial deployment. Generic automation platforms require customization and struggle with complex claims involving coverage disputes, multi-party liability, or state-specific requirements. Notch was purpose-built around insurance workflows for faster deployment and superior edge case handling.
Integration Depth and Scalability
Verify integration with actual technology stacks rather than accepting generic connectivity claims. Platforms executing actions in core systems enable straight-through processing, while read-only integrations deliver limited benefit despite appearing similar in demonstrations.
Time-to-Value and Support Model
Time-to-value and support model ensures that the duration from claim call to achieving an outcome stays as short as possible. It makes a difference between acknowledging the claim and delivering a solution, improving customer retention and satisfaction.
Common Misconceptions About Using AI Agents for Automated Ticket Resolution
The idea that AI can only handle simple cases comes from early chatbot limits and no longer fits modern agentic systems. Today’s platforms can manage complex workflows, from verifying coverage across policy types to handling multi-party claims and varying documentation rules.
Fears that automation hurts satisfaction usually reflect bad deflection tools, not true resolution. When AI solves issues faster and more accurately, satisfaction rises. And while DIY implementations can take six to twelve months, well-designed managed platforms can deliver results in 30 to 90 days.
Summary
FNOL is the highest-impact claims transformation opportunity available. The gap between current industry performance and achievable results is both a competitive opportunity and a risk. The best results come from resolution platforms rather than deflection ones, with deep system integration, and AI that understands how insurance works.
When evaluating options, focus on resolution rates, integration depth, insurance expertise, and commitments backed by actual guarantees. The technology to turn FNOL from a bottleneck to a launchpad exists right now.
Ready to see autonomous FNOL handling in action? Book a demo with Notch. The deal: 30% coverage within 90 days, and you pay nothing until that mark is hit.
Key Takeaways
- AI FNOL automation goes beyond data capture to automatically start claims, handling tasks like coverage checks, reserve setting, and adjuster assignment that once required human involvement.
- Modern platforms achieve 60-80% autonomous FNOL completion rates within 12 months of deployment, dramatically reducing cycle times while improving accuracy and customer satisfaction.
- Insurance-specific platforms deliver faster time-to-value than generic automation tools because they arrive pre-configured with policy structures, coverage logic, and regulatory requirements rather than requiring extensive customization.
- Integration depth determines real-world impact. Platforms that execute actions across policy admin, claims management, and payment systems enable true straight-through processing, while read-only integrations simply shift manual work downstream.
- Managed service implementations typically deliver results faster and with less organizational strain than DIY approaches, particularly for organizations without dedicated automation teams.
Got Questions? We’ve Got Answers
Notch guarantees 30% autonomous FNOL coverage within 90 days, with no cost until that mark is reached. Coverage rates typically climb to 60-80% autonomous completion within 12 months as systems learn from production volume.
Notch is different from other FNOL platforms because it’s purpose-built around insurance workflows, not generic automation. It offers faster deployment and superior coverage dispute handling, multi-party liability, and state-specific requirements. The platform executes actions across policy admin, claims management, and payment systems rather than just collecting data, and operates as a managed service rather than requiring internal configuration.
Yes, automated FNOL platforms detect fraud by analyzing patterns across submissions, identifying narrative inconsistencies, flagging duplicate claims or suspicious timing, and scoring fraud probability. Early detection prevents resource waste on fraudulent claims while pushing the legitimate ones to the top.
FNOL software handles emergency claims by using severity scoring to identify situations like bodily injury, total loss, or catastrophic events. Then, the platforms route the claims directly to senior adjusters or specialized teams while still capturing all intake data. This ensures critical cases receive immediate attention without sacrificing efficiency.














.png)
.png)

.png)



.jpg)

.png)


.jpg)

.png)






